
Does Insurance Cover Top Surgery?
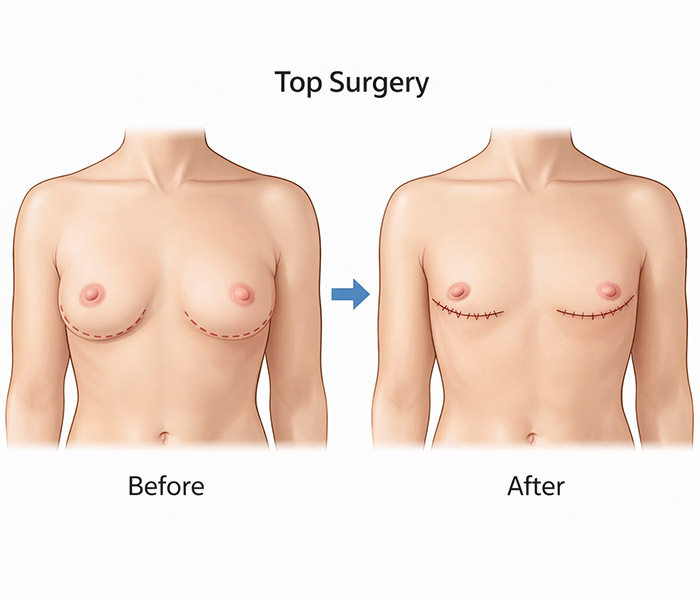
Top surgery refers to gender reassignment surgery procedure that involves the top half of your body. How much it costs depends on your insurance plan and whether your procedure is considered medically necessary. How much does top surgery cost with insurance? It depends.
Your coverage is determined by how your insurance defines medical necessity. If a doctor documents that the surgery is essential for your gender transition and mental health, your chances of getting your insurance to pay increase significantly.
Many New York insurance plans mandate coverage for gender reassignment surgery procedures, which may include:
- Male-to-female (MTF) top surgery, which may involve breast augmentation through implants
- Female-to-male (FTM) top surgery, which may involve breast reduction surgery
- Facial feminization surgery
- MTF bottom surgery
- FTM bottom surgery
Some insurance plans support gender-affirming surgery insurance coverage, while others only cover a percentage or nothing at all. Visit New York City’s Millennial Plastic Surgery, where an experienced team explains insurance policies clearly, so you don’t have to ask, “Does insurance cover gender-affirming surgery?” If you don’t have gender-affirming surgery insurance, they offer financing options to make the cost of your surgery manageable.
Is Top Surgery Covered by Insurance in New York City?
Many NYC insurers include top surgery insurance under their gender-affirming surgery insurance policy, as long as your medical documentation meets the plan guidelines. If you get your insurance through your employer, your coverage depends on whether your plan operates as fully insured or self-funded.
Large NYC insurance companies that frequently offer top surgery coverage include:
- Empire Blue Cross/Blue Shield, including Anthem-affiliated plans
- UnitedHealthcare
- Aetna
- Cigna
- Oscar Health
- Fidelis Care
- MetroPlus Health
- Medicaid-managed plans like Amida Care
- Medicare
Many of these insurers participate in the New York State of Health marketplace or offer employer-sponsored plans regulated under New York law. These plans include comprehensive transgender healthcare, such as surgical care tied to gender dysphoria. New York City provides strong legal protections, experienced surgeons and insurers knowledgeable about gender-affirming care.
When you pursue top surgery in NYC, advantages include:
- Broader insurer compliance with New York State law
- Well-defined medical procedures for necessary documentation
- Surgeons skilled in handling insurance approvals
 56 West 45th Street, 4th floor
56 West 45th Street, 4th floor New York, NY 10036 3190 Riverdale Ave. Level C #4A
Bronx, NY 10463 1000 Northern Blvd Suite 165
Great Neck, NY 11020

How Much Does Top Surgery Cost with Insurance?
Insurance companies in New York increasingly recognize top surgery as essential for gender-affirming care and so are paying for it. What may cost as much as $17,000 may only cost you several hundred or several thousand dollars, but many factors are at play. That’s great news if you’re asking, “Does insurance cover gender-affirming surgery?”
With the right documentation, your insurer covers a large portion of the procedure, but you may have additional costs to consider. Your deductible is the amount your insurance plan requires you to pay before coverage kicks in. You may also need to take care of the co-payment for your surgeon or facility visit on your own. Anesthesia and operating room fees sometimes fall outside your insurance coverage.
You may also need to pay for recovery-related items, such as:
- Compression garments
- Medications
- Follow-up appointments
- Post-surgical drains or dressings
- Specialized bras or binders for recovery
- Lab tests or imaging before or after surgery
- Recommended physical therapy or rehabilitation
Several other factors influence your final out-of-pocket costs, including the type of top surgery you choose. Your surgeon’s experience, reputation and specialization in gender-affirming procedures may also inflate your cost, but investing in an experienced surgeon like Dr. David Shokrian at Millennial Plastic Surgery ensures higher-quality results and safer outcomes.
What Documents Are Needed for Gender Reassignment Surgery Insurance Approval?
Your documentation helps insurance reviewers understand why top surgery addresses your medical needs. You usually need a letter from a licensed mental health professional, confirming that you’re experiencing gender dysphoria and explaining how top surgery supports your overall health. This doctor typically outlines your treatment history, states that you’re able to make an informed decision and explains why surgery fits into your care plan.
Your insurance also requests a letter from your surgeon or treating physician that explains the procedure, confirms that you’re ready for surgery and links your diagnosis to the planned surgical approach. This doctor may include relevant health history and physical findings to support the request.
Additional documents to complete the review process include:
- Supporting medical records. Your doctor’s notes show your treatment history and ongoing gender-affirming care.
- Hormone therapy documentation. Your records outline your hormone use and medical supervision, if your plan requires it.
- Prior authorization submission. Your surgeon’s office sends diagnosis codes, procedure details and supporting documents.
- Identification and insurance information. Your insurance card, photo ID and required member forms prevent delays.
Can Top Surgery Insurance Denials Be Appealed?
If your insurance denies coverage for your top surgery, you have the right to appeal the decision. You shouldn’t have to ask, “How does insurance cover top surgery?” It should be clear and straightforward, especially if you followed all the guidelines.
But denials often occur because:
- The insurance reviewer needs more proof that top surgery is medically necessary.
- You’ve submitted missing or incomplete documentation or unclear letters from your mental health provider or surgeon.
- There are plan-specific exclusions that you didn’t realize.
- Your submission contained administrative errors like incorrect codes or missing forms.
The appeal process usually involves several steps. Check each one to ensure your submission is as complete and thorough as possible. Most insurers set a timeframe for appeals, but let you request multiple levels if the first is denied.
The steps to follow include:
- Review your denial letter carefully to understand the reason for the rejection.
- Gather all necessary supporting documents, including letters from your mental health doctor and your surgeon, as well as any additional medical records.
- Have your surgeon clarify details and submit any additional documents.
- Make your appeal clear, detailed and easy to follow.
- Submit your appeal according to your insurer’s guidelines.
- Stay persistent, as many people gain approval through the appeals process.
How Do I Get Reimbursed for Top Surgery?
 How does health insurance cover gender-affirming surgery? Sometimes through reimbursements. Review your insurance policy to find the details under gender-affirming surgery insurance coverage, gender reassignment surgery insurance or top surgery insurance coverage. Learn what documentation is required and if there are any limits on coverage. Understand the deductibles and co-pays.
How does health insurance cover gender-affirming surgery? Sometimes through reimbursements. Review your insurance policy to find the details under gender-affirming surgery insurance coverage, gender reassignment surgery insurance or top surgery insurance coverage. Learn what documentation is required and if there are any limits on coverage. Understand the deductibles and co-pays.
New York insurance companies require you to provide timely, detailed documentation for reimbursement requests, including your:
- Receipts and invoices, such as surgery-related bills, facility fees, anesthesia, medications and recovery items
- Proof of payment, like bank statements, credit card statements or payment confirmations
- Medical letters, including documentation from your surgeon confirming the procedure and its medical necessity
- Prior authorization approval, if your plan requires it
- Insurance reimbursement forms, completed and signed
Submit your reimbursement request according to your insurer’s instructions. If your surgeon’s office offers claim assistance, take advantage of that service. Your request may take several weeks to process. Call your insurance provider for updates if you haven’t heard back within the expected timeframe, and respond promptly if they request additional paperwork. Is gender reassignment surgery covered by insurance in New York City? Yes, but you must do the work.
Why Should I Choose Millennial Plastic Surgery for Top Surgery?
The team at Millennial Plastic Surgery understands your goals and respects your identity. They know the questions to ask, like “Does insurance cover top surgery?” They navigate the insurance side of gender-affirming care.
Additionally, Dr. Shokrian stands out because he combines surgical expertise with real-world experience. He and his team help you through every step of the process, especially when you ask, “Does insurance cover gender-affirming surgery?” In New York, insurance rules are complex, and you may struggle with pre-authorizations, denials or confusing policy language.
The question to ask isn’t “How much does top surgery cost with insurance?” but instead, “Where can I get the best top surgery performed?” At Millennial Plastic Surgery, they prioritize safety and quality, as well as affordability. Dr. Shokrian operate in accredited facilities that follow strict surgical and post-operative care standards. Contact Millennial Plastic Surgery today for the most personalized gender reassignment surgery covered by insurance.

